Background
In September 2022, an outbreak of the Ebola Virus Disease (EVD) was declared in central Uganda. EVD is contagious and deadly, with an average case fatality rate of 50%, so containing the outbreak quickly was a matter of urgency. Uganda had already experienced previous EVD outbreaks in 2012 and 2019, and national health authorities–together with local and international partners–were able to draw on lessons learned from these outbreaks, use existing eIDSR systems–including DHIS2 as a platform and other tools–and leverage solutions developed to contain the COVID-19 pandemic to stop the 2022 EVD outbreak in its tracks.
“Uganda has shown that Ebola can be defeated when the whole system works together, from having an alert system in place, to finding and caring for people affected and their contacts, to gaining the full participation of affected communities in the response.”
Tedros Ghebreyesus, WHO Director-General.
Supporting Uganda’s EVD response with eIDSR and other tools
EVD (Sudan Variant) has no specific treatment and vaccines are still being developed. As such, management of the highly infectious disease involves palliative treatment of symptoms when detected early. Also, given that the early symptoms of EVD can be indistinguishable from those of diseases like malaria, which are endemic to the region, the need for an effective surveillance and case notification system was essential to halting the outbreak.
Uganda’s national disease surveillance and response organization is made up of several pillars that work together in response to prevent and control disease outbreaks. HISP Uganda supports the Strategic Information Research and Innovation (SIRI) pillar, which is responsible for innovation, data sharing and data use during the response. Other pillars include case management, surveillance (including Port of Entry and School-Based Surveillance), and lab (responsible for sample collection, testing and results). As part of the SIRI pillar, HISP Uganda and other partner’s task is to make sure that people in all pillars have the information they need and can make use of it at any time.
Effective disease surveillance in Uganda takes advantage of routine monitoring by District Health Team (DHTs) composed of Biostatistician, District Health Officer, District Surveillance Focal Persons (DSFPs), Health Sub-District Surveillance Focal Persons (HSDSFPs) and staff of health facilities and community engagements to track and report outbreaks. Disease surveillance data is aggregated and monitored at the district level by DHTs, who are also responsible for coordinating response activities within their respective districts such as case notification and investigation, monitoring and reporting in conjunction with the Regional and National Response Teams.
Following the country’s adoption of the revised guidelines on Integrated Disease Surveillance and Response (IDSR) in 2019, DHIS2 has been customised in Uganda as a national eIDSR system, which meant that the system was already in place when the COVID-19 pandemic started. HISP Uganda has supported the customisation, implementation and maintenance of the national eIDSR system. During the Pandemic, virtual trainings to DHTs were conducted for more than 90% of the districts within the country, helping build their capacity to use the eIDSR to respond to COVID-19 and other notifiable diseases for early detection. The eIDSR system provides DHTs with a single platform for alert management, Case Notification and Investigation and case management to avoid duplicate data entry and streamline the response.
The Ministry of Health Uganda leveraged this DHIS2-based eIDSR system to respond to the 2022 EVD outbreak, and–with technical and capacity building support from HISP Uganda–further refined the system for improved signal alert management, case notification and follow up, outbreak monitoring, and traveler screening.
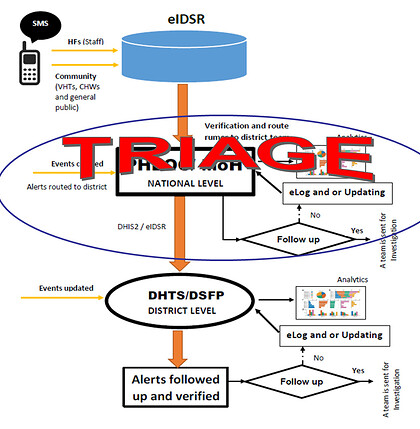
Signal alert management: SMS notification, triage and dispatch in DHIS2
One of the requirements of Uganda’s eIDSR is to have immediate notification from the community members to the district and national levels. In addition, there is a need to triage these alerts/signals to the districts so they are aware of what is happening within the districts, but ideally after the signal has been isolated from the noise.
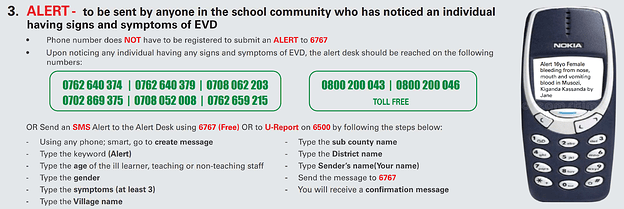
SMS Alert IEC
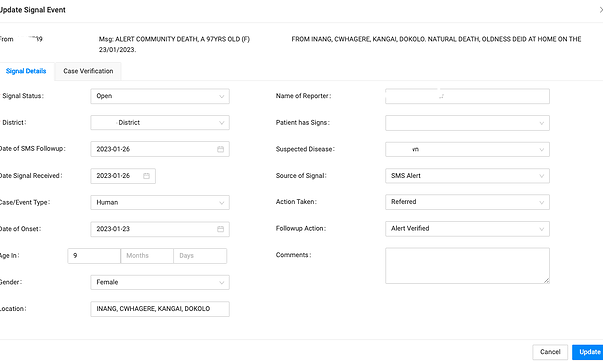
The eIDSR system in Uganda is based on DHIS2 version 2.35, which supports SMS functionality. The DHIS2 SMS Module implemented as part of the eIDSR enables immediate reporting of alerts/signals to national-level teams directly (and anonymously) from officials, community members, or health facilities at the community level. Each SMS is registered in DHIS2 (eIDSR) as an alert/signal event. Incoming alerts undergo a triage process, where they are reviewed in DHIS2 (eIDSR) at the national level, and the relevant ones forwarded to the districts for follow up.
SMS Alert management
During the EVD response, this workflow was adapted as call centers were set up in the 10 affected districts to support their response teams. These centers needed to manage and record any suspected cases that came through and to evacuate any that fit the EVD case definition. The SMS management app was modified by HISP Uganda to meet the needs of the response team. Within DHIS2 (eIDSR), call center workers could create a new Signal Event for an SMS or call, which would be verified by a separate team at the call center that could then send an ambulance in the case of a living patient displaying possible symptoms of EVD, or a dignified burial team for deceased cases. In the event of evacuation, an individual case would then be created in the Tracker program. In the end, most of the EVD alerts during the 2022 outbreak were logged via the call centers through this process.
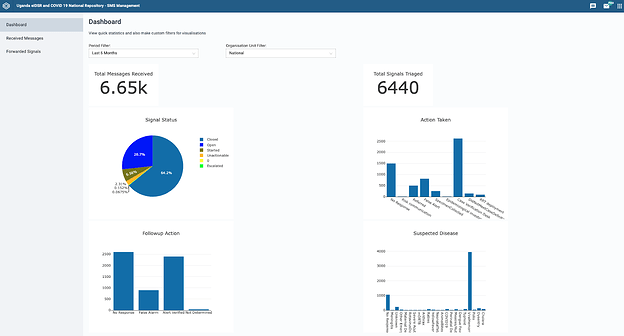
SMS Management Dashboard
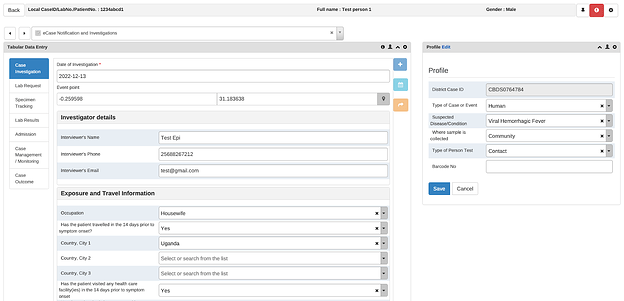
Case notification, investigation, admission and management in Tracker
The workflow for notification of a suspected case starts with the alert process above. As soon as an ambulance is dispatched by the call center to evacuate the individual, the district response team begins filling out the paper surveillance form, which needs to be completed in triplicate. One copy goes with the blood sample to the lab for testing, one with the patient to the designated health facility (Ebola Treatment Unit), and one is kept by the district health team. This last copy is used to enter the data into DHIS2 eIDSR, where it is used to create an individual record for the patient in the eCase Notification and Investigation Tracker program, which includes modules for case notification and investigation, Lab request and results, hospital admission and case management.
Ideally, by the time the lab results are ready, the case notification and investigation details have already been entered into the eIDSR by the DHT, so that the EVD treatment unit team at the health facility only needs to update the admission and case monitoring details for the case, followed by subsequent case management and monitoring information during the treatment period (this typically lasts 21-42 days for EVD cases), which they can do directly in the Tracker module. This helps save time for health workers and make data available more quickly to DHTs and national-level stakeholders.
The EVD Tracker also includes a module for lab results, and case outcomes–such as cured, transferred to another facility, deceased, and repatriated–are also recorded. Patients who have successfully recovered from EVD can be issued an electronic discharge certificate through DHIS2 eIDSR using a custom Discharge App developed by HISP Uganda (using a similar approach to the digital certificates developed during the COVID-19 pandemic). The goal of these printed certificates–which contain the patient’s name, ID number, discharging facility, and a scannable QR code–is to help people who have recovered from EVD to reintegrate into their communities by providing them with verifiable evidence of recovery, hopefully eliminating the stigma associated with EVD that has affected some survivors of previous outbreaks.
eIDSR Case Based Notification Tracker
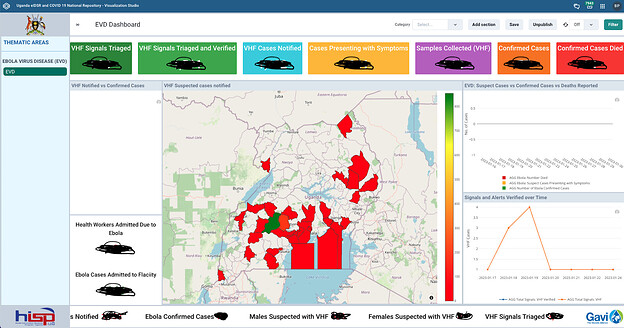
DHIS2 core and custom dashboards for monitoring EVD response
EVD Real time Dashboard
To support alert management, case monitoring and follow up, HISP Uganda configured a custom dashboard app for monitoring overall outbreak status. The dashboard keeps track of signals/alerts from SMS notifications as well as logs from the call center. It facilitates immediate notification to national-level teams and provides information necessary for triage, investigation, case management and contact tracing.
Meanwhile, the custom dashboard allows a variety of users and stakeholders to visualize cumulative data from the overall response in one place in a user-friendly format. This dashboard includes a map showing the geographic distribution of notified suspected cases; charts showing signals and alerts verified over time; and key indicators that reflect the full IDSR cascade, from the number of signals triaged and verified, to cases notified, cases presenting with symptoms, samples collected, confirmed cases, and deaths. Each pillar in the EVD response has access to these dashboards and is responsible for updating the eIDSR system with data from their pillar of responsibility.
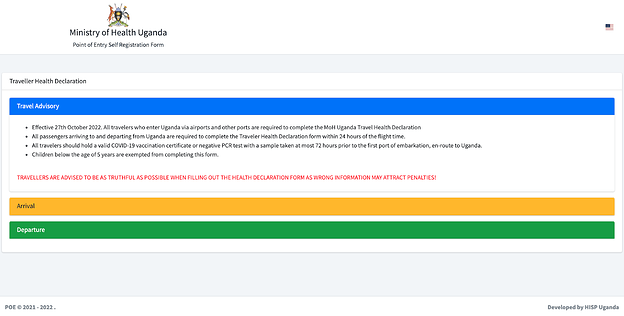
Port of entry screening and traveler self-reporting
PoE Self Declaration portal - https://poe-screening.health.go.ug/
During COVID-19, Uganda had implemented a PoE Tracker system to scan incoming travelers for infection. However, this system required significant resources, as the officials at the border needed to be equipped with mobile devices to scan and update individual traveler records, and high volume ports required significant a boost in the staffing (for example, a PoE with more 1,000 entries per day required around 20 staff members to handle individual traveler screening). This eventually proved to be unsustainable. To address this and prevent excessive travel delays at PoEs, HISP Uganda revised this system with input from the relevant PoE Sub-Pillar to allow border officials to submit aggregate reports instead of recording and updating each individual in Tracker. During that time, HISP Uganda also began work on a self-declaration form, that allowed travelers to self-screen for COVID-19 among other notifiable diseases and enter their own information in a secure web portal, generating a QR code that can be scanned by the Port Health Team at land, water and air crossings, creating a corresponding record in the eIDSR system.
For the EVD outbreak, HISP Uganda updated this self-declaration form to include new questions to help determine if travelers had recently been in an outbreak affected area, which was intended to be filled in both on arrival and departure. The updated design of the form allows it to be used for surveillance of notifiable diseases beyond EVD, so that the response teams can respond accordingly depending on the symptoms that travelers report. Some advantages to managing these records in the eIDSR system is that the DHIS2 can then be used to notify travelers of test results by SMS and email, and results can also be shared automatically with the respective pillars supporting the EVD response for prompt follow-up.
Additional surveillance tools developed by HISP Uganda
In addition to the digital systems and tools above, HISP Uganda worked to support two additional systems which, while not ultimately used in the 2022 EVD response, can further strengthen surveillance activities in the future:
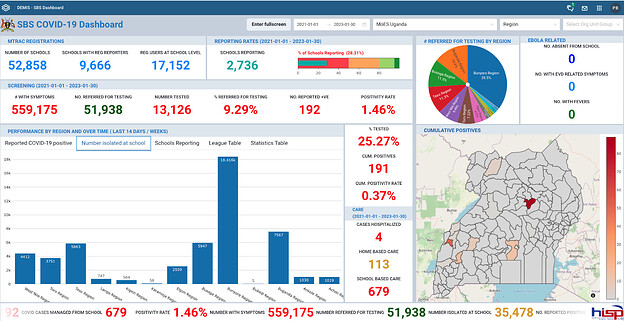
School-based surveillance (SBS) updated for EVD: During the COVID-19 pandemic, HISP Uganda implemented a School-Based Surveillance (SBS) system to support the safe reopening of Uganda’s schools following almost two years of closure. Using this system, school officials could report aggregate surveillance data directly into their DHIS2 for Education (DEMIS) system, along with other data used for education sector management, and the surveillance data would be automatically sent to the eIDSR system at the district level. From there, health officials could review the SBS dashboard and take appropriate action, including accessing the DEMIS system and drilling down to identify specific schools with significant incidences of symptoms and/or absences for follow up and support.
School Based Surveillance Real Time Dashboard with EVD data from schools
The EVD outbreak of 2022 began during the school year, and school-age children were among the early victims of the disease. At the request of the MoH, HISP Uganda worked to adapt the SBS system to support the EVD response by allowing the monitoring of the members of the school community who were displaying EVD symptoms or were repeatedly absent from school. School officials were also encouraged to make use of the alert system either by sending an SMS or calling the district call center alert desk. Ultimately, this system was not widely used during the EVD outbreak, as the government decided to close the schools and send learners home out of an abundance of caution. This system remains operational, and HISP Uganda is collaborating with MoH and MoES on proposals for general SBS strengthening, which could include monitoring other diseases beyond EVD and COVID-19.
Integrating GoData and DHIS2 for contact tracing: Contact tracing is an important part of EVD response, given the infectious nature of the disease. Typically, four contacts are investigated per suspected case. As the number of reported EVD cases increased, the number of potential contacts was expected to grow rapidly. To help manage this, the MoH decided to use Go.Data for contact tracing. Go.Data is an outbreak investigation tool for field data collection developed by the Global Outbreak and Response Network and coordinated by the WHO. The application had already been used Uganda prior to the 2022 EVD outbreak, but was not integrated with the eIDSR.
During the EVD response, HISP Uganda observed that many of the individual details captured within the contact tracing process are similar to those collected during case notification and investigation, leading to a desire to integrate Go.Data and DHIS2 to reduce duplicate work. However, while the forms used in Go.Data and Tracker were similar, there were some challenges in integrating them, notably the lack of a corresponding Organisation Unit structure in Go.Data, which made it difficult to associate Go.Data contacts and suspect cases with facilities and districts in DHIS2. This integration is still pending.
2022 EVD outbreak demonstrates utility of DHIS2 for eIDSR, and the need to continue strengthening the system
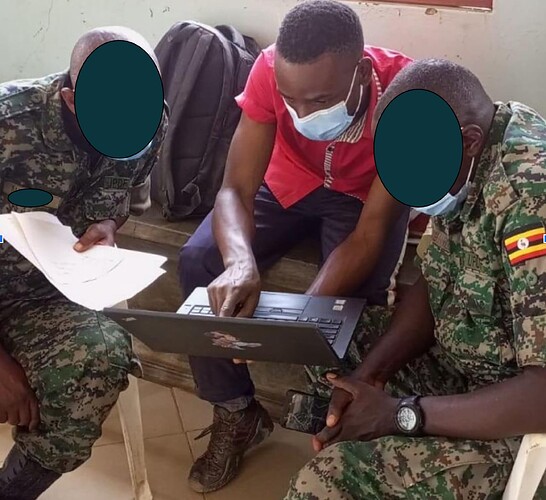
Training some of the Response Teams in eIDSR
Because of the lessons learned and successes using DHIS2 eIDSR for COVID-19 response, most districts supported the use of the eIDSR for EVD response to have all of the data in one system. At the beginning of the outbreak, HISP Uganda held refresher trainings for the district health teams, and the DHTs quickly started entering data in eIDSR. From September 2022 to January 2023, more than 1,000 suspected EVD cases were reported in the eIDSR.
During the course of the 2022 EVD outbreak, approximately 50% of confirmed EVD cases (77 of 146) were entered directly into the eIDSR. The missing 50% is due to the fact that the outbreak spread outside of the districts that were initially affected, where the support structures for collecting the EVD information in the eIDSR were not yet in place. HISP Uganda plans to work with these districts to enter the information from their paper or Excel files into DHIS2 eIDSR. To address this gap during the outbreak, the national surveillance team maintained a separate file that collated the information from these missing districts with the information from the eIDSR.
By the time the EVD outbreak was declared officially over on 11 January 2023, 55 people had died out of a total of 142 confirmed cases, including 19 healthcare workers. Additionally, 22 people died among probable cases without laboratory confirmation. Bringing the outbreak under control without greater loss of life required the combined effort of many partners using all of the tools at their disposal. Working together, these partners and systems helped the MoH Uganda contain the EVD outbreak within 3 months of the index case.